Vaccination
| Vaccinations | |
|---|---|
 Girl about to be vaccinated in her upper arm | |
| ICD-9-CM | 99.3-99.5 |
| Part of a series on |
| Vaccination |
|---|
Vaccination is the administration of a vaccine to help the immune system develop immunity from a disease. Vaccines contain a microorganism or virus in a weakened, live or killed state, or proteins or toxins from the organism. In stimulating the body's adaptive immunity, they help prevent sickness from an infectious disease. When a sufficiently large percentage of a population has been vaccinated, herd immunity results. Herd immunity protects those who may be immunocompromised and cannot get a vaccine because even a weakened version would harm them.[1] The effectiveness of vaccination has been widely studied and verified.[2][3][4] Vaccination is the most effective method of preventing infectious diseases;[5][6][7][8] widespread immunity due to vaccination is largely responsible for the worldwide eradication of smallpox and the elimination of diseases such as polio and tetanus from much of the world. According to the World Health Organization (WHO), vaccination prevents 3.5–5 million deaths per year.[9] A WHO-funded study by The Lancet estimates that, during the 50-year period starting in 1974, vaccination prevented 154 million deaths, including 146 million among children under age 5.[10] However, some diseases have seen rising cases due to relatively low vaccination rates attributable partly to vaccine hesitancy.[11]
The first disease people tried to prevent by inoculation was most likely smallpox, with the first recorded use of variolation occurring in the 16th century in China.[12] It was also the first disease for which a vaccine was produced.[13][14] Although at least six people had used the same principles years earlier, the smallpox vaccine was invented in 1796 by English physician Edward Jenner. He was the first to publish evidence that it was effective and to provide advice on its production.[15] Louis Pasteur furthered the concept through his work in microbiology. The immunization was called vaccination because it was derived from a virus affecting cows (Latin: vacca 'cow').[13][15] Smallpox was a contagious and deadly disease, causing the deaths of 20–60% of infected adults and over 80% of infected children.[16] When smallpox was finally eradicated in 1979, it had already killed an estimated 300–500 million people in the 20th century.[17][18][19]
Vaccination and immunization have a similar meaning in everyday language. This is distinct from inoculation, which uses unweakened live pathogens. Vaccination efforts have been met with some reluctance on scientific, ethical, political, medical safety, and religious grounds, although no major religions oppose vaccination, and some consider it an obligation due to the potential to save lives.[20] In the United States, people may receive compensation for alleged injuries under the National Vaccine Injury Compensation Program. Early success brought widespread acceptance, and mass vaccination campaigns have greatly reduced the incidence of many diseases in numerous geographic regions. The Centers for Disease Control and Prevention lists vaccination as one of the ten great public health achievements of the 20th century in the U.S.[21]
Mechanism of function
[edit]


Vaccines are a way of artificially activating the immune system to protect against infectious disease. The activation occurs through priming the immune system with an immunogen. Stimulating immune responses with an infectious agent is known as immunization. Vaccination includes various ways of administering immunogens.[22]
Most vaccines are administered before a patient has contracted a disease to help increase future protection. However, some vaccines are administered after the patient already has contracted a disease. Vaccines given after exposure to smallpox are reported to offer some protection from disease or may reduce the severity of disease.[23] The first rabies immunization was given by Louis Pasteur to a child after he was bitten by a rabid dog. Since its discovery, the rabies vaccine has been proven effective in preventing rabies in humans when administered several times over 14 days along with rabies immune globulin and wound care.[24] Other examples include experimental AIDS, cancer[25] and Alzheimer's disease vaccines.[26] Such immunizations aim to trigger an immune response more rapidly and with less harm than natural infection.[27]
Most vaccines are given by injection as they are not absorbed reliably through the intestines. Live attenuated polio, rotavirus, some typhoid, and some cholera vaccines are given orally to produce immunity in the bowel. While vaccination provides a lasting effect, it usually takes several weeks to develop. This differs from passive immunity (the transfer of antibodies, such as in breastfeeding), which has immediate effect.[28]
A vaccine failure is when an organism contracts a disease in spite of being vaccinated against it. Primary vaccine failure occurs when an organism's immune system does not produce antibodies when first vaccinated. Vaccines can fail when several series are given and fail to produce an immune response. The term "vaccine failure" does not necessarily imply that the vaccine is defective. Most vaccine failures are simply due to individual variations in immune response.[29]
Vaccination versus inoculation
[edit]The term "inoculation" is often used interchangeably with "vaccination." However, while related, the terms are not synonymous. Vaccination is treatment of an individual with an attenuated (i.e. less virulent) pathogen or other immunogen, whereas inoculation, also called variolation in the context of smallpox prophylaxis, is treatment with unattenuated variola virus taken from a pustule or scab of a smallpox patient into the superficial layers of the skin, commonly the upper arm. Variolation was often done 'arm-to-arm' or, less effectively, 'scab-to-arm', and often caused the patient to become infected with smallpox, which in some cases resulted in severe disease.[30][31]
Vaccinations began in the late 18th century with the work of Edward Jenner and the smallpox vaccine.[32][33][34]
Preventing disease versus preventing infection
[edit]Some vaccines, like the smallpox vaccine, prevent infection. Their use results in sterilizing immunity and can help eradicate a disease if there is no animal reserve. Other vaccines, including those for COVID-19, help to (temporarily) lower the chance of severe disease for individuals, without necessarily reducing the probability of becoming infected.[35]
Safety
[edit]
Vaccine development and approval
[edit]Just like any medication or procedure, no vaccine can be 100% safe or effective for everyone because each person's body can react differently.[36][37] While minor side effects, such as soreness or low grade fever, are relatively common, serious side effects are very rare and occur in about 1 out of every 100,000 vaccinations and typically involve allergic reactions that can cause hives or difficulty breathing.[38][39]
However, vaccines are the safest they ever have been in history and each vaccine undergoes rigorous clinical trials to ensure their safety and efficacy before approval by authorities such as the US Food and Drug Administration (FDA).[40]
Prior to human testing, vaccines are tested on cell cultures and the results modelled to assess how they will interact with the immune system.[38][40] During the next round of testing, researchers study vaccines in animals, including mice, rabbits, guinea pigs, and monkeys.[38] Vaccines that pass each of these stages of testing are then approved by the public health safety authority (FDA in the United States) to start a three-phase series of human testing, advancing to higher phases only if they are deemed safe and effective at the previous phase. The people in these trials participate voluntarily and are required to prove they understand the purpose of the study and the potential risks.[40]
During phase I trials, a vaccine is tested in a group of about 20 people with the primary goal of assessing the vaccine's safety.[38] Phase II trials expand the testing to include 50 to several hundred people. During this stage, the vaccine's safety continues to be evaluated and researchers also gather data on the effectiveness and the ideal dose of the vaccine.[38] Vaccines determined to be safe and efficacious then advance to phase III trials, which focuses on the efficacy of the vaccine in hundreds to thousands of volunteers. This phase can take several years to complete and researchers use this opportunity to compare the vaccinated volunteers to those who have not been vaccinated to highlight any true reactions to the vaccine that occur.[40]
If a vaccine passes all of the phases of testing, the manufacturer can then apply for license of the vaccine through the relevant regulatory authorities such as the FDA in US. Before regulatory authorities approve use in the general public, they extensively review the results of the clinical trials, safety tests, purity tests, and manufacturing methods and establish that the manufacturer itself is up to government standards in many other areas.[38][41]
After regulatory approval, the regulators continue to monitor the manufacturing protocols, batch purity, and the manufacturing facility itself. Additionally, vaccines also undergo phase IV trials, which monitor the safety and efficacy of vaccines in tens of thousands of people, or more, across many years.[38][41]
Side effects
[edit]The Centers for Disease Control and Prevention (CDC) has compiled a list of vaccines and their possible side effects.[39] The risk of side effects varies between vaccines.
Notable vaccine investigations
[edit]In 1976 in the United States, a mass swine flu vaccination programme was discontinued after 362 cases of Guillain–Barré syndrome among 45 million vaccinated people. William Foege of the CDC estimated that the incidence of Guillain-Barré was four times higher in vaccinated people than in those not receiving the swine flu vaccine.
Dengvaxia, the only approved vaccine for Dengue fever, was found to increase the risk of hospitalization for Dengue fever by 1.58 times in children of 9 years or younger, resulting in the suspension of a mass vaccination program in the Philippines in 2017.[42]
Pandemrix – a vaccine for the H1N1 pandemic of 2009 given to around 31 million people[37] – was found to have a higher level of adverse events than alternative vaccines resulting in legal action.[43] In a response to the narcolepsy reports following immunization with Pandemrix, the CDC carried out a population-based study and found the FDA-approved 2009 H1N1 flu shots were not associated with an increased risk for the neurological disorder.[44]
Ingredients
[edit]The ingredients of vaccines can vary greatly from one to the next and no two vaccines are the same. The CDC has compiled a list of vaccines and their ingredients that is readily accessible on their website.[45]
Aluminium
[edit]Aluminium is an adjuvant ingredient in some vaccines. An adjuvant is a type of ingredient that is used to help the body's immune system create a stronger immune response after receiving the vaccination.[46] Aluminium is in a salt form (the ionic version of an element) and is used in the following compounds: aluminium hydroxide, aluminium phosphate, and aluminium potassium sulfate. For a given element, the ion form has different properties from the elemental form. Although it is possible to have aluminium toxicity, aluminium salts have been used effectively and safely since the 1930s when they were first used with the diphtheria and tetanus vaccines.[46] Although there is a small increase in the chance of having a local reaction to a vaccine with an aluminium salt (redness, soreness, and swelling), there is no increased risk of any serious reactions.[47][48]
Mercury
[edit]Certain vaccines once contained a compound called thiomersal or thimerosal, which is an organic compound containing mercury. Organomercury is commonly found in two forms. The methylmercury cation (with one carbon atom) is found in mercury-contaminated fish and is the form that people might ingest in mercury-polluted areas (Minamata disease), whereas the ethylmercury cation (with two carbon atoms) is present in thimerosal, linked to thiosalicylate.[49] Although both are organomercury compounds, they do not have the same chemical properties and interact with the human body differently. Ethylmercury is cleared from the body faster than methylmercury and is less likely to cause toxic effects.[49]
Thimerosal was used as a preservative to prevent the growth of bacteria and fungi in vials that contain more than one dose of a vaccine.[49] This helps reduce the risk of potential infections or serious illness that could occur from contamination of a vaccine vial. Although there was a small increase in risk of injection site redness and swelling with vaccines containing thimerosal, there was no increased risk of serious harm or autism.[50][51] Even though evidence supports the safety and efficacy of thimerosal in vaccines, thimerosal was removed from childhood vaccines in the United States in 2001 as a precaution.[49]
Monitoring
[edit]CDC Immunization Safety Office initiatives[52]
Vaccine Adverse Event Reporting System (VAERS)[53] |Food and Drug Administration (FDA) Center for Biologics Evaluation and Research (CBER)[54] |Immunization Action Coalition (IAC)[55]
Vaccine Safety Datalink (VSD)[56] |Health Resources and Service Administration (HRSA)[57] |Institute for Safe Medication Practices (ISMP)[58]
Clinical Immunization Safety Assessment (CISA) Project National Institutes of Health (NIH)[59]
National Vaccine Program Office (NVPO)[60]
The administration protocols, efficacy, and adverse events of vaccines are monitored by organizations of the US federal government, including the CDC and FDA, and independent agencies are constantly re-evaluating vaccine practices.[52][61] As with all medications, vaccine use is determined by public health research, surveillance, and reporting to governments and the public.[52][61]
Usage
[edit]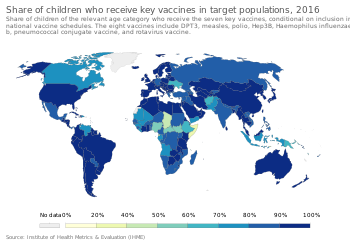

The World Health Organization (WHO) has estimated that vaccination prevents 3.5–5 million deaths per year,[9] and up to 1.5 million children die each year due to diseases that could have been prevented by vaccination.[64] They estimate that 29% of deaths of children under five-years-old in 2013 were vaccine preventable. In other developing parts of the world, they are faced with the challenge of having a decreased availability of resources and vaccinations. Countries such as those in Sub-Saharan Africa cannot afford to provide the full range of childhood vaccinations.[65]
In 2024, a WHO/UNICEF report found “the number of children who received three doses of the vaccine against diphtheria, tetanus and pertussis (DTP) in 2023 – a key marker for global immunization coverage – stalled at 84% (108 million). However, the number of children who did not receive a single dose of the vaccine increased from 13.9 million in 2022 to 14.5 million in 2023. More than half of unvaccinated children live in the 31 countries with fragile, conflict-affected and vulnerable settings.”[66]
United States
[edit]Vaccines have led to major decreases in the prevalence of infectious diseases in the United States. In 2007, studies regarding the effectiveness of vaccines on mortality or morbidity rates of those exposed to various diseases found almost 100% decreases in death rates, and about a 90% decrease in exposure rates.[67] Vaccination adoption is reduced among some populations, such as those with low incomes, people with limited access to health care, and members of certain racial and ethnic minorities. Distrust of health-care providers, language barriers, and misleading or false information also contribute to lower adoption, as does anti-vaccine activism.[68]
Most government and private health insurance plans cover recommended vaccines at no charge when received by providers in their networks.[69] The federal Vaccines for Children Program and the Social Security Act are among the major sources of financial support for vaccination of those in lower-income groups.[70][71]
The Centers for Disease Control and Prevention (CDC) publishes uniform national vaccine recommendations and immunization schedules, although state and local governments, as well as nongovernmental organizations, may have their own policies.[72]
History
[edit]
Before the first vaccinations, in the sense of using cowpox to inoculate people against smallpox, people have been inoculated in China and elsewhere, before being copied in the west, by using smallpox, called variolation. The earliest hints of the practice of variolation for smallpox in China come during the 10th century.[73] The Chinese also practiced the oldest documented use of variolation, which comes from Wan Quan's (1499–1582) Douzhen Xinfa (痘疹心法) of 1549. They implemented a method of "nasal insufflation" administered by blowing powdered smallpox material, usually scabs, up the nostrils. Various insufflation techniques have been recorded throughout the sixteenth and seventeenth centuries within China.[74]: 60 Two reports on the Chinese practice of inoculation were received by the Royal Society in London in 1700; one by Martin Lister who received a report by an employee of the East India Company stationed in China and another by Clopton Havers.[75] In France, Voltaire reports that the Chinese have practiced variolation "these hundred years".
In 1796, Edward Jenner, a doctor in Berkeley in Gloucestershire, England, tested a common theory that a person who had contracted cowpox would be immune from smallpox. To test the theory, he took cowpox vesicles from a milkmaid named Sarah Nelmes with which he infected an eight-year-old boy named James Phipps, and two months later he inoculated the boy with smallpox, and smallpox did not develop. In 1798, Jenner published An Inquiry Into the Causes and Effects of the Variolæ Vaccinæ which created widespread interest. He distinguished 'true' and 'spurious' cowpox (which did not give the desired effect) and developed an "arm-to-arm" method of propagating the vaccine from the vaccinated individual's pustule. Early attempts at confirmation were confounded by contamination with smallpox, but despite controversy within the medical profession and religious opposition to the use of animal material, by 1801 his report was translated into six languages and over 100,000 people were vaccinated.[76] The term vaccination was coined in 1800 by the surgeon Richard Dunning in his text Some observations on vaccination.[77]

In 1802, the Scottish physician Helenus Scott vaccinated dozens of children in Bombay against smallpox using Jenner's cowpox vaccine.[81] In the same year Scott penned a letter to the editor in the Bombay Courier, declaring that "We have it now in our power to communicate the benefits of this important discovery to every part of India, perhaps to China and the whole eastern world".[82]: 243 Subsequently, vaccination became firmly established in British India. A vaccination campaign was started in the new British colony of Ceylon in 1803. By 1807 the British had vaccinated more than a million Indians and Sri Lankans against smallpox.[82]: 244 Also in 1803 the Spanish Balmis Expedition launched the first transcontinental effort to vaccinate people against smallpox.[83] Following a smallpox epidemic in 1816 the Kingdom of Nepal ordered smallpox vaccine and requested the English veterinarian William Moorcroft to help in launching a vaccination campaign.[82]: 265–266 In the same year a law was passed in Sweden to require the vaccination of children against smallpox by the age of two. Prussia briefly introduced compulsory vaccination in 1810 and again in the 1920s, but decided against a compulsory vaccination law in 1829. A law on compulsory smallpox vaccination was introduced in the Province of Hanover in the 1820s. In 1826, in Kragujevac, future prince Mihailo of Serbia was the first person to be vaccinated against smallpox in the principality of Serbia.[84] Following a smallpox epidemic in 1837 that caused 40,000 deaths, the British government initiated a concentrated vaccination policy, starting with the Vaccination Act of 1840, which provided for universal vaccination and prohibited variolation.[82]: 365 The Vaccination Act 1853 introduced compulsory smallpox vaccination in England and Wales.[85]: 39 The law followed a severe outbreak of smallpox in 1851 and 1852. It provided that the poor law authorities would continue to dispense vaccination to all free of charge, but that records were to be kept on vaccinated children by the network of births registrars.[85]: 41 It was accepted at the time, that voluntary vaccination had not reduced smallpox mortality,[85]: 43 but the Vaccination Act 1853 was so badly implemented that it had little impact on the number of children vaccinated in England and Wales.[85]: 50
The U.S. Supreme Court upheld compulsory vaccination laws in the 1905 landmark case Jacobson v. Massachusetts, ruling that laws could require vaccination to protect the public from dangerous communicable diseases. However, in practice the U.S. had the lowest rate of vaccination among industrialized nations in the early 20th century. Compulsory vaccination laws began to be enforced in the U.S. after World War II. In 1959, the WHO called for the eradication of smallpox worldwide, as smallpox was still endemic in 33 countries. In the 1960s six to eight children died each year in the U.S. from vaccination-related complications. According to the WHO there were in 1966 about 100 million cases of smallpox worldwide, causing an estimated two million deaths. In the 1970s there was such a small risk of contracting smallpox that the U.S. Public Health Service recommended for routine smallpox vaccination to be ended. By 1974 the WHO smallpox vaccination program had confined smallpox to parts of Pakistan, India, Bangladesh, Ethiopia and Somalia. In 1977 the WHO recorded the last case of smallpox infection acquired outside a laboratory in Somalia. In 1980 the WHO officially declared the world free of smallpox.[86]: 115–116
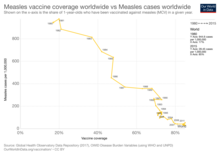
In 1974 the WHO adopted the goal of universal vaccination by 1990 to protect children against six preventable infectious diseases: measles, poliomyelitis, diphtheria, whooping cough, tetanus, and tuberculosis.[86]: 119 In the 1980s only 20 to 40% of children in developing countries were vaccinated against these six diseases. In wealthy nations the number of measles cases had dropped dramatically after the introduction of the measles vaccine in 1963. WHO figures demonstrate that in many countries a decline in measles vaccination leads to a resurgence in measles cases. Measles are so contagious that public health experts believe a vaccination rate of 100% is needed to control the disease.[86]: 120 Despite decades of mass vaccination polio remains a threat in India, Nigeria, Somalia, Niger, Afghanistan, Bangladesh and Indonesia. By 2006 global health experts concluded that the eradication of polio was only possible if the supply of drinking water and sanitation facilities were improved in slums.[86]: 124 The deployment of a combined DPT vaccine against diphtheria, pertussis (whooping cough), and tetanus in the 1950s was considered a major advancement for public health. But in the course of vaccination campaigns that spanned decades, DPT vaccines became associated with large number of cases with side effects. Despite improved DPT vaccines coming onto the market in the 1990s DPT vaccines became the focus of anti-vaccination campaigns in wealthy nations. As immunization rates fell outbreaks of pertussis increased in many countries.[86]: 128
In 2000, the Global Alliance for Vaccines and Immunization was established to strengthen routine vaccinations and introduce new and underused vaccines in countries with a per capita GDP of under US$1000.[87]
UNICEF has reported on the extent to which children missed out on vaccinations from 2020 onwards due to the COVID-19 pandemic. By summer 2023, the organisation described vaccination programs as getting "back on track".[88]
Vaccination policy
[edit]
To eliminate the risk of outbreaks of some diseases, at various times governments and other institutions have employed policies requiring vaccination for all people. For example, an 1853 law required universal vaccination against smallpox in England and Wales, with fines levied on people who did not comply.[89] Common contemporary U.S. vaccination policies require that children receive recommended vaccinations before entering public school.[90]
Beginning with early vaccination in the nineteenth century, these policies were resisted by a variety of groups, collectively called antivaccinationists, who object on scientific, ethical, political, medical safety, religious, and other grounds.[91] Common objections are that vaccinations do not work, that compulsory vaccination constitutes excessive government intervention in personal matters, or that the proposed vaccinations are not sufficiently safe.[92] Many modern vaccination policies allow exemptions for people who have compromised immune systems, allergies to the components used in vaccinations or strongly held objections.[93]
In countries with limited financial resources, limited vaccination coverage results in greater morbidity and mortality due to infectious disease.[94] More affluent countries are able to subsidize vaccinations for at-risk groups, resulting in more comprehensive and effective coverage. In Australia, for example, the Government subsidizes vaccinations for seniors and indigenous Australians.[95]
Public Health Law Research, an independent US based organization, reported in 2009 that there is insufficient evidence to assess the effectiveness of requiring vaccinations as a condition for specified jobs as a means of reducing incidence of specific diseases among particularly vulnerable populations;[96] that there is sufficient evidence supporting the effectiveness of requiring vaccinations as a condition for attending child care facilities and schools;[97] and that there is strong evidence supporting the effectiveness of standing orders, which allow healthcare workers without prescription authority to administer vaccine as a public health intervention.[98]
Fractional dose vaccination
[edit]Fractional dose vaccination reduces the dose of a vaccine to allow more individuals to be vaccinated with a given vaccine stock, trading societal benefit for individual protection. Based on the nonlinearity properties of many vaccines, it is effective in poverty diseases[99] and promises benefits in pandemic waves, e.g. in COVID-19,[100] when vaccine supply is limited.
Litigation
[edit]Allegations of vaccine injuries in recent decades have appeared in litigation in the U.S. Some families have won substantial awards from sympathetic juries, even though most public health officials have said that the claims of injuries were unfounded.[101] In response, several vaccine makers stopped production, which the US government believed could be a threat to public health, so laws were passed to shield manufacturers from liabilities stemming from vaccine injury claims.[101] The safety and side effects of multiple vaccines have been tested to uphold the viability of vaccines as a barrier against disease. The influenza vaccine was tested in controlled trials and proven to have negligible side effects equal to that of a placebo.[102] Some concerns from families might have arisen from social beliefs and norms that cause them to mistrust or refuse vaccinations, contributing to this discrepancy in side effects that were unfounded.[103]
Opposition
[edit]
Opposition to vaccination, from a wide array of vaccine critics, has existed since the earliest vaccination campaigns.[92] It is widely accepted that the benefits of preventing serious illness and death from infectious diseases greatly outweigh the risks of rare serious adverse effects following immunization.[105] Some studies have claimed to show that current vaccine schedules increase infant mortality and hospitalization rates;[106][107] those studies, however, are correlational in nature and therefore cannot demonstrate causal effects, and the studies have also been criticized for cherry picking the comparisons they report, for ignoring historical trends that support an opposing conclusion, and for counting vaccines in a manner that is "completely arbitrary and riddled with mistakes".[108][109]
Various disputes have arisen over the morality, ethics, effectiveness, and safety of vaccination. Some vaccination critics say that vaccines are ineffective against disease[110] or that vaccine safety studies are inadequate.[110] Some religious groups do not allow vaccination,[111] and some political groups oppose mandatory vaccination on the grounds of individual liberty.[92] In response, concern has been raised that spreading unfounded information about the medical risks of vaccines increases rates of life-threatening infections, not only in the children whose parents refused vaccinations, but also in those who cannot be vaccinated due to age or immunodeficiency, who could contract infections from unvaccinated carriers (see herd immunity).[112] Some parents believe vaccinations cause autism, although there is no scientific evidence to support this idea.[113] In 2011, Andrew Wakefield, a leading proponent of the theory that MMR vaccine causes autism, was found to have been financially motivated to falsify research data and was subsequently stripped of his medical license.[114] In the United States people who refuse vaccines for non-medical reasons have made up a large percentage of the cases of measles, and subsequent cases of permanent hearing loss and death caused by the disease.[115]
Many parents do not vaccinate their children because they feel that diseases are no longer present due to vaccination.[116] This is a false assumption, since diseases held in check by immunization programs can and do still return if immunization is dropped. These pathogens could possibly infect vaccinated people, due to the pathogen's ability to mutate when it is able to live in unvaccinated hosts.[117][118]
Vaccination and autism
[edit]The notion of a connection between vaccines and autism originated in a 1998 paper published in The Lancet whose lead author was the physician Andrew Wakefield. His study concluded that eight of the 12 patients, ages 3 years to 10 years, developed behavioral symptoms consistent with autism following the MMR vaccine (an immunization against measles, mumps, and rubella).[119] The article was widely criticized for lack of scientific rigor and it was proven that Wakefield falsified data in the article.[119] In 2004, 10 of the original 12 co-authors (not including Wakefield) published a retraction of the article and stated the following: "We wish to make it clear that in this paper no causal link was established between MMR vaccine and autism as the data were insufficient."[120] In 2010, The Lancet officially retracted the article, stating that several elements of the article were incorrect, including falsified data and protocols. The article has sparked a much greater anti-vaccination movement, particularly in the United States, and even though the article was shown to be fraudulent and was heavily retracted, one in four parents still believe that vaccines can cause autism.[121]
To date, all validated and definitive studies have shown that there is no correlation between vaccines and autism.[122] One of the studies published in 2015 confirms there is no link between autism and the MMR vaccine. Infants were given a health plan, that included an MMR vaccine, and were continuously studied until they reached five years old. There was no link between the vaccine and children who had a normally developed sibling or a sibling that had autism making them a higher risk for developing autism themselves.[123]
It can be difficult to correct the memory of humans when wrong information is received prior to correct information. Even though there is much evidence to go against the Wakefield study and retractions were published by most of the co-authors, many people continue to believe and base decisions on the study as it still lingers in their memory. Studies and research are being conducted to determine effective ways to correct misinformation in the public memory.[124]
Routes of administration
[edit]A vaccine administration may be oral, by injection (intramuscular, intradermal, subcutaneous), by puncture, transdermal or intranasal.[125] Several recent clinical trials have aimed to deliver the vaccines via mucosal surfaces to be up-taken by the common mucosal immunity system, thus avoiding the need for injections.[126]
Economics of vaccination
[edit]Health is often used as one of the metrics for determining the economic prosperity of a country. This is because healthier individuals are generally better suited to contributing to the economic development of a country than the sick.[127] There are many reasons for this. For instance, a person who is vaccinated for influenza not only protects themselves from the risk of influenza, but simultaneously also prevents themselves from infecting those around them.[128] This leads to a healthier society, which allows individuals to be more economically productive. Children are consequently able to attend school more often and have been shown to do better academically. Similarly, adults are able to work more often, more efficiently, and more effectively.[127][129]
Costs and benefits
[edit]On the whole, vaccinations induce a net benefit to society. Vaccines are often noted for their high Return on investment (ROI) values, especially when considering the long-term effects.[130] Some vaccines have much higher ROI values than others. Studies have shown that the ratios of vaccination benefits to costs can differ substantially—from 27:1 for diphtheria/pertussis, to 13.5:1 for measles, 4.76:1 for varicella, and 0.68–1.1 : 1 for pneumococcal conjugate.[128] Some governments choose to subsidize the costs of vaccines, due to some of the high ROI values attributed to vaccinations. The United States subsidizes over half of all vaccines for children, which costs between $400 and $600 each. Although most children do get vaccinated, the adult population of the US is still below the recommended immunization levels. Many factors can be attributed to this issue. Many adults who have other health conditions are unable to be safely immunized, whereas others opt not to be immunized for the sake of private financial benefits. Many Americans are underinsured, and, as such, are required to pay for vaccines out-of-pocket. Others are responsible for paying high deductibles and co-pays. Although vaccinations usually induce long-term economic benefits, many governments struggle to pay the high short-term costs associated with labor and production. Consequently, many countries neglect to provide such services.[128]
According to a 2021 paper, vaccinations against haemophilus influenzae type b, hepatitis B, human papillomavirus, Japanese encephalitis, measles, neisseria meningitidis serogroup A, rotavirus, rubella, streptococcus pneumoniae, and yellow fever have prevented an estimated 50 million deaths from 2000 to 2019.[131] The paper "represents the largest assessment of vaccine impact before COVID-19-related disruptions".[131] According to a June 2022 study, COVID‑19 vaccinations prevented an additional 14.4 to 19.8 million deaths in 185 countries and territories from 8 December 2020 to 8 December 2021.[132][133]
They estimated that it would cost between $2.8 billion and $3.7 billion to develop at least one vaccine for each of them. This should be set against the potential cost of an outbreak. The 2003 SARS outbreak in East Asia cost $54 billion.[134]
Game theory uses utility functions to model costs and benefits, which may include financial and non-financial costs and benefits. In recent years, it has been argued that game theory can effectively be used to model vaccine uptake in societies. Researchers have used game theory for this purpose to analyse vaccination uptake in the context of diseases such as influenza and measles.[135]
Gallery
[edit]-
Dr Jenner performing his first vaccination on James Phipps, a boy of age 8. 14 May 1796. Painting by Ernest Board (early 20th century)
-
James Gillray's The Cow-Pock—or—the Wonderful Effects of the New Inoculation!, an 1802 caricature of vaccinated patients who feared it would make them sprout cowlike appendages
-
La vaccine or Le préjugé vaincu by Louis-Léopold Boilly, 1807
-
A doctor vaccinating a small girl, other girls with loosened blouses wait their turn apprehensively by Lance Calkin
-
German caricature showing von Behring extracting the serum with a tap
-
Les Malheurs de la Vaccine (The history of vaccination seen from an economic point of view: A pharmacy up for sale; an outmoded inoculist selling his premises; Jenner, to the left, pursues a skeleton with a lancet)
See also
[edit]References
[edit]- ^ "Herd immunity (Herd protection) | Vaccine Knowledge". vk.ovg.ox.ac.uk. Archived from the original on 2 August 2019. Retrieved 12 November 2020.
- ^ Fiore AE, Bridges CB, Cox J (2009). "Seasonal Influenza Vaccines". Vaccines for Pandemic Influenza. Current Topics in Microbiology and Immunology. Vol. 333. pp. 43–82. doi:10.1007/978-3-540-92165-3_3. ISBN 978-3-540-92164-6. PMID 19768400. S2CID 33549265.
- ^ Chang Y, Brewer NT, Rinas AC, Schmitt K, Smith JS (July 2009). "Evaluating the impact of human papillomavirus vaccines". Vaccine. 27 (32): 4355–62. doi:10.1016/j.vaccine.2009.03.008. PMID 19515467.
- ^ Liesegang TJ (August 2009). "Varicella zoster virus vaccines: effective, but concerns linger". Canadian Journal of Ophthalmology. 44 (4): 379–84. doi:10.3129/i09-126. PMID 19606157.
- ^ A CDC framework for preventing infectious diseases (PDF). United States Centers for Disease Control and Prevention. October 2011. Archived from the original (PDF) on 14 September 2012.
Vaccines are our most effective and cost-saving tools for disease prevention, preventing untold suffering and saving tens of thousands of lives and billions of dollars in healthcare costs each year
- ^ Gellin B (1 June 2000). "Vaccines and Infectious Diseases: Putting Risk into Perspective". American Medical Association Briefing on Microbial Threats. National Press Club Washington, DC. Archived from the original on 24 November 2010.
Vaccines are the most effective public health tool ever created.
- ^ "Vaccine-preventable diseases". Public Health Agency of Canada. 7 October 2002. Archived from the original on 24 March 2012.
Vaccines still provide the most effective, longest-lasting method of preventing infectious diseases in all age groups
- ^ "NIAID Biodefense Research Agenda for Category B and C Priority Pathogens" (PDF). United States National Institute of Allergy and Infectious Diseases (NIAID). Archived from the original (PDF) on 4 March 2016.
Vaccines are the most effective method of protecting the public against infectious diseases.
- ^ a b "Vaccines and immunization". World Health Organization. Archived from the original on 1 January 2022. Retrieved 18 September 2022.
- ^ "Vaccines and immunization". The Lancet. 403 (10441): 2307–2316. 25 May 2024.
- ^ "Editorial: Global Health Concerns as Vaccine-Preventable Infections Including SARS-CoV-2 (JN.1), Influenza, Respiratory Syncytial Virus (RSV), and Measles Continue to Rise". 1 February 2024.
- ^ Williams 2010, p. 60.
- ^ a b Lombard M, Pastoret PP, Moulin AM (April 2007). "A brief history of vaccines and vaccination". Revue Scientifique et Technique. 26 (1): 29–48. doi:10.20506/rst.26.1.1724. PMID 17633292. S2CID 6688481.
- ^ Behbehani AM (December 1983). "The smallpox story: life and death of an old disease". Microbiological Reviews. 47 (4): 455–509. doi:10.1128/MMBR.47.4.455-509.1983. PMC 281588. PMID 6319980.
- ^ a b Plett PC (2006). "[Peter Plett and other discoverers of cowpox vaccination before Edward Jenner]". Sudhoffs Archiv (in German). 90 (2): 219–32. PMID 17338405. Archived from the original on 15 February 2008. Retrieved 12 March 2008.
- ^ Riedel S (January 2005). "Edward Jenner and the history of smallpox and vaccination". Proceedings. 18 (1): 21–5. doi:10.1080/08998280.2005.11928028. PMC 1200696. PMID 16200144.
- ^ Koplow DA (2003). Smallpox: the fight to eradicate a global scourge. Berkeley: University of California Press. ISBN 978-0-520-24220-3.
- ^ "UC Davis Magazine, Summer 2006: Epidemics on the Horizon". Archived from the original on 11 December 2008. Retrieved 3 January 2008.
- ^ "How Poxviruses Such As Smallpox Evade The Immune System". ScienceDaily. Archived from the original on 28 February 2020. Retrieved 17 October 2023.
- ^ McNeil DG (26 April 2019). "Religious Objections to the Measles Vaccine? Get the Shots, Faith Leaders Say". The New York Times. Archived from the original on 28 April 2019. Retrieved 29 April 2019.
- ^ CDC (April 1999). "Ten great public health achievements--United States, 1900-1999". MMWR. Morbidity and Mortality Weekly Report. 48 (12): 241–3. PMID 10220250. Archived from the original on 11 July 2011. Retrieved 16 April 2022.
- ^ Kwong PD (November 2017). "What Are the Most Powerful Immunogen Design Vaccine Strategies? A Structural Biologist's Perspective". Cold Spring Harbor Perspectives in Biology. 9 (11): a029470. doi:10.1101/cshperspect.a029470. PMC 5666634. PMID 28159876.
- ^ "Vaccine Overview" (PDF). Smallpox Fact Sheet. Archived from the original (PDF) on 2 January 2008. Retrieved 2 January 2008.
- ^ Rupprecht CE, Briggs D, Brown CM, Franka R, Katz SL, Kerr HD, et al. (March 2010). "Use of a reduced (4-dose) vaccine schedule for postexposure prophylaxis to prevent human rabies: recommendations of the advisory committee on immunization practices". MMWR. Recommendations and Reports. 59 (RR-2): 1–9. PMID 20300058.
- ^ Oppenheimer SB, Alvarez M, Nnoli J (2008). "Carbohydrate-based experimental therapeutics for cancer, HIV/AIDS and other diseases". Acta Histochemica. 110 (1): 6–13. doi:10.1016/j.acthis.2007.08.003. PMC 2278011. PMID 17963823.
- ^ Goñi F, Sigurdsson EM (February 2005). "New directions towards safer and effective vaccines for Alzheimer's disease". Current Opinion in Molecular Therapeutics. 7 (1): 17–23. PMID 15732525.
- ^ Irvine DJ, Swartz MA, Szeto GL (November 2013). "Engineering synthetic vaccines using cues from natural immunity". Nature Materials. 12 (11): 978–90. Bibcode:2013NatMa..12..978I. doi:10.1038/nmat3775. PMC 3928825. PMID 24150416.
- ^ "Immunity Types". Centers for Disease Control and Prevention. Archived from the original on 22 December 2011. Retrieved 20 October 2015.
- ^ Wiedermann U, Garner-Spitzer E, Wagner A (2016). "Primary vaccine failure to routine vaccines: Why and what to do?". Human Vaccines & Immunotherapeutics. 12 (1): 239–43. doi:10.1080/21645515.2015.1093263. PMC 4962729. PMID 26836329.
- ^ "The Smallpox Epidemic of 1862 (Victoria BC)--Doctors and Diagnosis". web.uvic.ca. Archived from the original on 2 February 2018. Retrieved 29 September 2016.
- ^ "Doctors and diagnosis The difference between Vaccination and Inoculation". Web.uvic.ca. Archived from the original on 2 February 2018. Retrieved 8 January 2014.
- ^ "Edward Jenner – (1749–1823)". Sundaytimes.lk. 1 June 2008. Archived from the original on 26 September 2011. Retrieved 28 July 2009.
- ^ "History – Edward Jenner (1749–1823)". BBC. Archived from the original on 8 March 2021. Retrieved 1 March 2014.
- ^ "Edward Jenner – Smallpox and the Discovery of Vaccination". dinweb.org. Archived from the original on 27 August 2010. Retrieved 22 April 2010.
- ^ Caddy, Sarah L. (5 January 2021). "Coronavirus: few vaccines prevent infection – here's why that's not a problem". The Conversation. Archived from the original on 18 December 2022. Retrieved 18 December 2022.
- ^ "History of Vaccine Safety History Ensuring Safety Vaccine Safety CDC". www.cdc.gov. 10 January 2019. Archived from the original on 28 March 2019. Retrieved 12 March 2019.
- ^ a b Chen RT, Hibbs B (July 1998). "Vaccine safety: current and future challenges". Pediatric Annals. 27 (7): 445–55. doi:10.3928/0090-4481-19980701-11. PMID 9677616. S2CID 13364842.
- ^ a b c d e f g "Making Safe Vaccines NIH: National Institute of Allergy and Infectious Diseases". www.niaid.nih.gov. Archived from the original on 28 March 2019. Retrieved 12 March 2019.
- ^ a b "Vaccines: Vac-Gen/Side Effects". www.cdc.gov. 12 July 2018. Archived from the original on 17 March 2017. Retrieved 12 March 2019.
- ^ a b c d "Ensuring Vaccine Safety Ensuring Safety Vaccine Safety CDC". www.cdc.gov. 12 December 2018. Archived from the original on 12 March 2019. Retrieved 12 March 2019.
- ^ a b "How are vaccines developed? WHO". www.who.int. 8 December 2020. Archived from the original on 26 October 2023. Retrieved 26 October 2023.
- ^ Redoni M, Yacoub S, Rivino L, Giacobbe DR, Luzzati R, Di Bella S (July 2020). "Dengue: Status of current and under-development vaccines". Reviews in Medical Virology. 30 (4): e2101. doi:10.1002/rmv.2101. hdl:1983/6d38d9b6-8e1b-4a84-85e3-edab4fc41957. PMID 32101634. S2CID 211536962. Archived from the original on 20 March 2022. Retrieved 23 September 2021.
- ^ Doshi, Peter (20 September 2018). "Pandemrix vaccine: why was the public not told of early warning signs?". BMJ. 362: k3948. doi:10.1136/bmj.k3948. PMID 30237282. S2CID 52308748.
- ^ "Narcolepsy Following Pandemrix in Europe". www.cdc.gov. 20 August 2020. Archived from the original on 27 June 2016. Retrieved 3 January 2021.
- ^ "Vaccines: Vac-Gen/Additives in Vaccines Fact Sheet". www.cdc.gov. 12 July 2018. Archived from the original on 30 May 2019. Retrieved 15 March 2019.
- ^ a b "Adjuvants help vaccines work better. Vaccine Safety CDC". www.cdc.gov. 23 January 2019. Archived from the original on 15 March 2019. Retrieved 15 March 2019.
- ^ Jefferson T, Rudin M, Di Pietrantonj C (February 2004). "Adverse events after immunisation with aluminium-containing DTP vaccines: systematic review of the evidence". The Lancet. Infectious Diseases. 4 (2): 84–90. doi:10.1016/S1473-3099(04)00927-2. PMID 14871632.
- ^ Mitkus RJ, King DB, Hess MA, Forshee RA, Walderhaug MO (November 2011). "Updated aluminum pharmacokinetics following infant exposures through diet and vaccination". Vaccine. 29 (51): 9538–43. doi:10.1016/j.vaccine.2011.09.124. PMID 22001122.
- ^ a b c d "Thimerosal in Vaccines Thimerosal Concerns Vaccine Safety CDC". www.cdc.gov. 24 January 2019. Archived from the original on 17 August 2011. Retrieved 22 March 2019.
- ^ Ball LK, Ball R, Pratt RD (May 2001). "An assessment of thimerosal use in childhood vaccines". Pediatrics. 107 (5): 1147–54. doi:10.1542/peds.107.5.1147. PMID 11331700.
- ^ "Vaccine Safety & Availability - Thimerosal and Vaccines". www.fda.gov. Archived from the original on 6 January 2013. Retrieved 22 March 2019.
- ^ a b c "Vaccine Safety Monitoring Monitoring Ensuring Safety Vaccine Safety CDC". www.cdc.gov. 12 December 2018. Archived from the original on 30 March 2019. Retrieved 24 March 2019.
- ^ "Vaccine Adverse Event Reporting System (VAERS)". vaers.hhs.gov. Archived from the original on 17 March 2019. Retrieved 24 March 2019.
- ^ "About the Center for Biologics Evaluation and Research (CBER)". www.fda.gov. 7 February 2019. Archived from the original on 9 May 2017. Retrieved 24 March 2019.
- ^ "Immunization Action Coalition (IAC): Vaccine Information for Health Care Professionals". www.immunize.org. Archived (PDF) from the original on 14 December 2017. Retrieved 24 March 2019.
- ^ "Vaccine Safety Datalink (VSD) VSD Monitoring Ensuring Safety Vaccine Safety CDC". www.cdc.gov. 10 January 2019. Archived from the original on 30 March 2019. Retrieved 24 March 2019.
- ^ "Official web site of the U.S. Health Resources & Services Administration". www.hrsa.gov. Archived from the original on 23 March 2019. Retrieved 24 March 2019.
- ^ "Home". Institute For Safe Medication Practices. Archived from the original on 20 March 2022. Retrieved 24 March 2019.
- ^ "National Institutes of Health (NIH)". National Institutes of Health (NIH). Archived from the original on 2 October 2019. Retrieved 24 March 2019.
- ^ "National Vaccine Program Office (NVPO)". HHS.gov. 30 March 2016. Archived from the original on 24 March 2019. Retrieved 24 March 2019.
- ^ a b "Vaccine safety, surveillance and reporting". Government of Canada. 22 April 2014. Archived from the original on 13 April 2020. Retrieved 14 April 2020.
- ^ "Share of children who receive key vaccines in target populations". Our World in Data. Archived from the original on 5 May 2020. Retrieved 5 March 2020.
- ^ "Global vaccination coverage". Our World in Data. Archived from the original on 3 July 2020. Retrieved 5 March 2020.
- ^ "Global Immunization Data" (PDF). Archived (PDF) from the original on 13 April 2020. Retrieved 5 October 2020.
- ^ Ehreth J (January 2003). "The global value of vaccination". Vaccine. 21 (7–8): 596–600. doi:10.1016/S0264-410X(02)00623-0. PMID 12531324.
- ^ "Global childhood immunization levels stalled in 2023, leaving many without life-saving protection". www.who.int. Retrieved 20 July 2024.
- ^ Roush SW, Murphy TV (November 2007). "Historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States". JAMA. 298 (18): 2155–63. doi:10.1001/jama.298.18.2155. PMID 18000199.
- ^ Hill, Holly A. (2024). "Decline in Vaccination Coverage by Age 24 Months and Vaccination Inequities Among Children Born in 2020 and 2021 — National Immunization Survey-Child, United States, 2021–2023". MMWR. Morbidity and Mortality Weekly Report. 73. doi:10.15585/mmwr.mm7338a3. ISSN 0149-2195.
- ^ "How to pay for vaccines". 10 July 2024.
- ^ "Vaccines for Children Program (VFC)". CDC. 2 April 2019. Archived from the original on 1 May 2020. Retrieved 8 December 2019.
- ^ "Program for Distribution of Pediatric Vaccines". Social Security. U.S. Government. Archived from the original on 30 October 2019. Retrieved 8 December 2019.
- ^ "Who Calls the Shots? A Legal and Historical Perspective on Vaccine Mandates". 7 September 2022.
- ^ Needham J (2000). Science and Civilisation in China: Volume 6, Biology and Biological Technology, Part 6, Medicine. Cambridge University Press. p. 154. ISBN 9780521632621.
- ^ Williams G (2010). Angel of Death. Basingstoke c: Palgrave Macmillan. ISBN 978-0-230-27471-6.
- ^ Silverstein AM (2009). A History of Immunology (2nd ed.). Academic Press. p. 293. ISBN 9780080919461.
- ^ Gross CP, Sepkowitz KA (July 1998). "The myth of the medical breakthrough: smallpox, vaccination, and Jenner reconsidered". International Journal of Infectious Diseases. 3 (1): 54–60. doi:10.1016/s1201-9712(98)90096-0. PMID 9831677.
- ^ Dunning R (1800). "Some observations on vaccination, or, The inoculated cow-pox; Some observations on vaccination; Inoculated cow-pox; Observations, & c; Observations, &c". Contagion – CURIOSity Digital Collections. March and Teape. Archived from the original on 18 March 2020. Retrieved 2 April 2020.
- ^ Sethu, Divya (16 March 2021). "How 3 Mysore Queens Became The Face Of A Campaign For The World's First Vaccine". The Better India. Archived from the original on 22 March 2023. Retrieved 26 October 2022.
- ^ "An Indian Queen's "Vaccine Selfie" in Oils". www.gavi.org. Archived from the original on 15 March 2023. Retrieved 26 October 2022.
- ^ "The Indian queens who modelled for the world's first vaccine". BBC News. 19 September 2020. Archived from the original on 20 September 2020. Retrieved 26 October 2022.
- ^ Foege WH (2011). House on Fire: The Fight to Eradicate Smallpox. University of California Press. p. 92. ISBN 978-0-520-26836-4.
- ^ a b c d Bennett M (2016). The War Against Smallpox: Edward Jenner and the Global Spread of Vaccination. Cambridge University Press. ISBN 9780521765671.
- ^ "Exhibition tells story of Spanish children used as vaccine fridges in 1803". the Guardian. 27 July 2021. Archived from the original on 3 September 2021. Retrieved 31 July 2021.
- ^ "Prvo vakcinisanje u Kragujevcu". Archived from the original on 8 March 2022. Retrieved 17 May 2021.
- ^ a b c d Brunton D (2008). The Politics of Vaccination: Practice and Policy in England, Wales, Ireland, and Scotland, 1800-1874. University Rochester Press. ISBN 9781580460361.
- ^ a b c d e f Magner LN (2009). A History of Infectious Diseases and the Microbial World. ABC-CLIO. ISBN 9780275995058.
- ^ Jaupart P, Dipple L, Dercon S (3 December 2019). "Has Gavi lived up to its promise? Quasi-experimental evidence on country immunisation rates and child mortality". BMJ Global Health. 3 (4): e001789. doi:10.1136/bmjgh-2019-001789. PMC 6936423. PMID 31908857.
- ^ UNICEF UK, Child Matters, Summer 2023, pp. 10-11
- ^ Brunton D (2008). The Politics of Vaccination: Practice and Policy in England, Wales, Ireland, and Scotland, 1800–1874. University of Rochester Press. p. 39.
- ^ "State Vaccination Requirements". CDC. 11 March 2019. Archived from the original on 2 April 2020. Retrieved 7 December 2019.
- ^ Tolley K (May 2019). "School Vaccination Wars". History of Education Quarterly. 59 (2): 161–194. doi:10.1017/heq.2019.3.
- ^ a b c Wolfe RM, Sharp LK (August 2002). "Anti-vaccinationists past and present". BMJ. 325 (7361): 430–2. doi:10.1136/bmj.325.7361.430. PMC 1123944. PMID 12193361.
- ^ Salmon DA, Teret SP, MacIntyre CR, Salisbury D, Burgess MA, Halsey NA (February 2006). "Compulsory vaccination and conscientious or philosophical exemptions: past, present, and future". Lancet. 367 (9508): 436–42. doi:10.1016/S0140-6736(06)68144-0. PMID 16458770. S2CID 19344405.
- ^ Mhatre SL, Schryer-Roy AM (October 2009). "The fallacy of coverage: uncovering disparities to improve immunization rates through evidence. Results from the Canadian International Immunization Initiative Phase 2 – Operational Research Grants". BMC International Health and Human Rights. 9 (S1): S1. doi:10.1186/1472-698X-9-S1-S1. PMC 3226229. PMID 19828053.
- ^ "Time to think about vaccinations again?". Medicines Talk (No. 32 Summer 2009). Sydney, Australia: NPS MedicineWise. 1 February 2010. Archived from the original on 27 July 2011.
- ^ "Laws and Policies Requiring Specified Vaccinations among High Risk Populations". Public Health Law Research. 7 December 2009. Archived from the original on 18 November 2017. Retrieved 19 November 2014.
- ^ "Vaccination Requirements for Child Care, School and College Attendance". Public Health Law Research. 12 July 2009. Archived from the original on 18 November 2017. Retrieved 19 November 2014.
- ^ "Standing Orders for Vaccination". Public Health Law Research. 12 July 2009. Archived from the original on 18 November 2017. Retrieved 8 January 2014.
- ^ Nelson, Katherine S.; Janssen, Julia M.; Troy, Stephanie B.; Maldonado, Yvonne (5 January 2012). "Intradermal fractional dose inactivated polio vaccine: A review of the literature". Vaccine. 30 (2): 121–125. doi:10.1016/j.vaccine.2011.11.018. ISSN 0264-410X. PMID 22100886. Archived from the original on 26 January 2022. Retrieved 18 August 2021.
- ^ Hunziker P (24 July 2021). "Personalized-dose Covid-19 vaccination in a wave of virus Variants of Concern: Trading individual efficacy for societal benefit". Precision Nanomedicine. 4 (3): 805–820. doi:10.33218/001c.26101. Archived from the original on 9 October 2021. Retrieved 18 August 2021.
- ^ a b Sugarman SD (September 2007). "Cases in vaccine court—legal battles over vaccines and autism". The New England Journal of Medicine. 357 (13): 1275–7. doi:10.1056/NEJMp078168. PMID 17898095.
- ^ Nichol KL, Margolis KL, Lind A, Murdoch M, McFadden R, Hauge M, Magnan S, Drake M (July 1996). "Side effects associated with influenza vaccination in healthy working adults. A randomized, placebo-controlled trial". Archives of Internal Medicine. 156 (14): 1546–50. doi:10.1001/archinte.1996.00440130090009. PMID 8687262.
- ^ Oraby T, Thampi V, Bauch CT (April 2014). "The influence of social norms on the dynamics of vaccinating behaviour for paediatric infectious diseases". Proceedings. Biological Sciences. 281 (1780): 20133172. doi:10.1098/rspb.2013.3172. PMC 4078885. PMID 24523276.
- ^ Larson HJ, de Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IG, Cook AR, Jones NS (October 2016). "The State of Vaccine Confidence 2016: Global Insights Through a 67-Country Survey". eBioMedicine. 12: 295–301. doi:10.1016/j.ebiom.2016.08.042. PMC 5078590. PMID 27658738.
- ^ Bonhoeffer J, Heininger U (June 2007). "Adverse events following immunization: perception and evidence". Current Opinion in Infectious Diseases. 20 (3): 237–46. doi:10.1097/QCO.0b013e32811ebfb0. PMID 17471032. S2CID 40669829.
- ^ Miller NZ, Goldman GS (September 2011). "Infant mortality rates regressed against number of vaccine doses routinely given: is there a biochemical or synergistic toxicity?". Human & Experimental Toxicology. 30 (9): 1420–8. doi:10.1177/0960327111407644. PMC 3170075. PMID 21543527.
- ^ Goldman GS, Miller NZ (October 2012). "Relative trends in hospitalizations and mortality among infants by the number of vaccine doses and age, based on the Vaccine Adverse Event Reporting System (VAERS), 1990–2010". Human & Experimental Toxicology. 31 (10): 1012–21. doi:10.1177/0960327112440111. PMC 3547435. PMID 22531966.
- ^ Science Mom, Catherina (9 May 2011). "Infant mortality and vaccines". Just The Vax. Blogspot.com. Archived from the original on 10 October 2019. Retrieved 10 October 2019.
- ^ Miller, N.; Goldman, G. (2011). "Infant mortality rates regressed against number of vaccine doses routinely given: Is there a biochemical or synergistic toxicity?". Human & Experimental Toxicology. 30 (9): 1420–1428. doi:10.1177/0960327111407644. ISSN 0960-3271. PMC 3170075. PMID 21543527. Archived from the original on 26 January 2022. Retrieved 10 October 2019.
- ^ a b Halvorsen R (2007). The Truth about Vaccines. Gibson Square. ISBN 978-1-903933-92-3.
- ^ Sinal SH, Cabinum-Foeller E, Socolar R (July 2008). "Religion and medical neglect". Southern Medical Journal. 101 (7): 703–6. doi:10.1097/SMJ.0b013e31817997c9. PMID 18580731. S2CID 29738930.
- ^ Omer SB, Salmon DA, Orenstein WA, deHart MP, Halsey N (May 2009). "Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases". The New England Journal of Medicine. 360 (19): 1981–8. doi:10.1056/NEJMsa0806477. PMID 19420367. S2CID 5353949.
- ^ Gross L (May 2009). "A broken trust: lessons from the vaccine--autism wars". PLOS Biology. 7 (5): e1000114. doi:10.1371/journal.pbio.1000114. PMC 2682483. PMID 19478850.
- ^ "Retracted autism study an 'elaborate fraud,' British journal finds". CNN.com. 6 January 2011. Archived from the original on 4 January 2018. Retrieved 26 April 2013.
- ^ Phadke VK, Bednarczyk RA, Salmon DA, Omer SB (March 2016). "Association Between Vaccine Refusal and Vaccine-Preventable Diseases in the United States: A Review of Measles and Pertussis". JAMA. 315 (11): 1149–58. doi:10.1001/jama.2016.1353. PMC 5007135. PMID 26978210.
- ^ "WHO – World Immunization Week 2012". who.int. Archived from the original on 21 September 2013.
- ^ Inglis-Arkell E (January 2014). "Why anti-vaxxers might be creating a world of more dangerous viruses". io9. Archived from the original on 13 July 2019. Retrieved 10 June 2019.
- ^ "Pertussis and Other Diseases Could Return If Vaccination Rates Lag". ContagionLive. 26 March 2019. Archived from the original on 26 March 2019. Retrieved 10 June 2019.
- ^ a b Wakefield AJ, Murch SH, Anthony A, Linnell J, Casson DM, Malik M, Berelowitz M, Dhillon AP, Thomson MA, Harvey P, Valentine A, Davies SE, Walker-Smith JA (February 1998). "Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children". Lancet. 351 (9103): 637–41. doi:10.1016/S0140-6736(97)11096-0. PMID 9500320. S2CID 439791. Archived from the original on 27 September 2007. Retrieved 5 February 2012. (Retracted, see doi:10.1016/S0140-6736(10)60175-4, PMID 20137807, Retraction Watch)
- ^ Murch SH, Anthony A, Casson DH, Malik M, Berelowitz M, Dhillon AP, Thomson MA, Valentine A, Davies SE, Walker-Smith JA (March 2004). "Retraction of an interpretation". Lancet. 363 (9411): 750. doi:10.1016/S0140-6736(04)15715-2. PMID 15016483. S2CID 5128036.
- ^ Daley MF, Glanz JM (September 2011). "Straight talk about vaccination". Scientific American. 305 (3): 32–34. Bibcode:2011SciAm.305b..32D. doi:10.1038/scientificamerican0911-32. PMID 21870438.
- ^ "Vaccines Do Not Cause Autism Concerns Vaccine Safety CDC". www.cdc.gov. 6 February 2019. Archived from the original on 16 March 2017. Retrieved 22 March 2019.
- ^ Jain A, Marshall J, Buikema A, Bancroft T, Kelly JP, Newschaffer CJ (April 2015). "Autism occurrence by MMR vaccine status among US children with older siblings with and without autism". JAMA. 313 (15): 1534–40. doi:10.1001/jama.2015.3077. PMID 25898051.
- ^ Pluviano S, Watt C, Della Sala S (27 July 2017). "Misinformation lingers in memory: Failure of three pro-vaccination strategies". PLOS ONE. 12 (7): e0181640. Bibcode:2017PLoSO..1281640P. doi:10.1371/journal.pone.0181640. PMC 5547702. PMID 28749996.
- ^ Plotkin SA (2006). Mass Vaccination: Global Aspects – Progress and Obstacles (Current Topics in Microbiology & Immunology). Springer-Verlag Berlin and Heidelberg GmbH & Co. K. ISBN 978-3-540-29382-8.
- ^ Fujkuyama Y, Tokuhara D, Kataoka K, Gilbert RS, McGhee JR, Yuki Y, Kiyono H, Fujihashi K (March 2012). "Novel vaccine development strategies for inducing mucosal immunity". Expert Review of Vaccines. 11 (3): 367–79. doi:10.1586/erv.11.196. PMC 3315788. PMID 22380827.
- ^ a b Quilici S, Smith R, Signorelli C (12 August 2015). "Role of vaccination in economic growth". Journal of Market Access & Health Policy. 3: 27044. doi:10.3402/jmahp.v3.27044. PMC 4802686. PMID 27123174.
- ^ a b c Institute of Medicine; Board on Health Care Services; Committee on the Evaluation of Vaccine Purchase Financing in the United States (10 December 2003). Financing Vaccines in the 21st Century. doi:10.17226/10782. ISBN 978-0-309-08979-1. PMID 25057673. Archived from the original on 20 March 2022. Retrieved 6 February 2019.
- ^ "The Economic Side of Vaccines' Positive Externalities". Econlife. 24 February 2015. Archived from the original on 8 September 2018. Retrieved 7 September 2018.
- ^ Carroll S, Rojas AJ, Glenngård AH, Marin C (12 August 2015). "Vaccination: short- to long-term benefits from investment". Journal of Market Access & Health Policy. 3: 27279. doi:10.3402/jmahp.v3.27279. PMC 4802682. PMID 27123171.
- ^ a b Toor, Jaspreet; Echeverria-Londono, Susy; Li, Xiang; Abbas, Kaja; Carter, Emily D; Clapham, Hannah E; Clark, Andrew; de Villiers, Margaret J; Eilertson, Kirsten; Ferrari, Matthew; Gamkrelidze, Ivane (13 July 2021). Stanley, Margaret; Harper, Diane M; Soldan, Kate (eds.). "Lives saved with vaccination for 10 pathogens across 112 countries in a pre-COVID-19 world". eLife. 10: e67635. doi:10.7554/eLife.67635. ISSN 2050-084X. PMC 8277373. PMID 34253291.
- ^ Watson OJ, Barnsley G, Toor J, Hogan AB, Winskill P, Ghani AC (June 2022). "Global impact of the first year of COVID-19 vaccination: a mathematical modelling study". The Lancet Infectious Diseases. 22 (9): 1293–1302. doi:10.1016/s1473-3099(22)00320-6. PMC 9225255. PMID 35753318.
- ^ "COVID-19 vaccines saved nearly 20 million lives in a year, study says". CBS News. 24 June 2022. Archived from the original on 29 June 2022. Retrieved 27 June 2022.
- ^ "Scientists have estimated the cost of stopping 11 diseases that could kill millions in a pandemic". Vox. 22 October 2018. Archived from the original on 6 November 2018. Retrieved 2 December 2018.
- ^ Chang SL, Piraveenan M, Pattison P, Prokopenko M (December 2020). "Game theoretic modelling of infectious disease dynamics and intervention methods: a review". Journal of Biological Dynamics. 14 (1): 57–89. arXiv:1901.04143. doi:10.1080/17513758.2020.1720322. PMID 31996099. S2CID 58004680.
Further reading
[edit]- Carroll AE (17 September 2015). "Not Up for Debate: The Science Behind Vaccination". The New York Times. Archived from the original on 7 February 2019. Retrieved 6 February 2019.
- Cole JP, Swendiman KS (21 May 2014). "Mandatory Vaccinations: Precedent and Current Laws" (PDF). Congressional Research Service. Archived (PDF) from the original on 9 August 2021. Retrieved 31 January 2020.
- Largent MA (2012). Vaccine: The Debate in Modern America. Baltimore: Johns Hopkins University Press. ISBN 978-1-4214-0607-7.
- Offit, Paul A. (12 June 2007). Vaccinated. Harper Collins. ISBN 978-0-06-122795-0.
- Williams G (2010). Angel of Death. Basingstoke: Palgrave Macmillan. ISBN 978-0230274716.
- Walloch KL (2015). The Antivaccine Heresy: Jacobson v. Massachusetts and the Troubled History of Compulsory Vaccination in the United States. University of Rochester Press. p. xii.
External links
[edit]- U.S. government Vaccine Research Center: Information regarding preventive vaccine research studies
- The Vaccine Page links to resources in many countries.
- "The complete routine immunisation schedule from summer 2014". Published by the UK Department of Health. (PDF)
- National Immunization Program, US Centers for Disease Control
- "Vaccine Safety" – US Centers for Disease Control
- "Vaccines Timeline" – Centers for Disease Control and Prevention
- Immunize.org – Immunization Action Coalition' (nonprofit working to increase immunization rates)
- WHO.int – 'Immunizations, vaccines and biologicals: Towards a World free of Vaccine Preventable Diseases', World Health Organization (WHO's global vaccination campaign website)
- Health-EU Portal Vaccinations in the EU
- History of Vaccines Medical education site from the College of Physicians of Philadelphia, the oldest medical professional society in the US
- Images of vaccine-preventable diseases
- Immunisation, BBC Radio 4 discussion with Nadja Durbach, Chris Dye & Sanjoy Bhattacharya (In Our Time, 20 April 2006)






